The Life Link Clinic
Background
The Cheshire and Merseyside Rehabilitation Network works in collaboration with various NHS Trusts and Local Authorities in Merseyside, providing complex rehabilitation inpatient and community services for patients who have experienced major traumatic life events such as brain injuries and/or have long term conditions resulting in cognitive impairment or physical disabilities. These injuries can have a dramatic impact on the patient’s quality of life; affecting employment, housing, finances as well as having an impact on their families (1).
Patients and families within the complex rehabilitation units have indicated a lack of access to coordinated socioeconomic support for non-medical issues such as finance and housing needs resulting in increased stress and anxiety. Services offered to patients and their families have shown to be disconnected, lack individualism and are often reactive in nature, resulting in poorer outcomes (2). This is coupled with the fact that Knowsley, an area most users of the service reside in, is one of the most deprived areas in England and Liverpool having a ranking of 3rd most deprived in terms health deprivation and disability (3).
In October 2017, in response to feedback from patients and families, the Life Link clinic was set up. The clinic is a collaborative one-stop drop-in service supported by the NHS, Local Authorities and the Brain Charity to help tackle some of the health inequalities experienced by the users of complex inpatient rehabilitation services, offering advice and support on socioeconomic issues.

Who is affected by the problem?
Patients who have experienced neurological trauma and their families. Patients with neurological traumas or long-term neurological conditions have the worst outcomes of all other long-term conditions (4) and there is also evidence to suggest that there is increased incidence of traumatic brain injury in individuals living in more deprived areas (5)
Who was involved in the research and how were they involved?
In addition to staff members, two public advisors were involved as part of the project management team. The public advisors were previous patients on the complex rehabilitation inpatient unit and resided in the Merseyside area, one of whom was a carer and therefore had experience from a carer’s perspective of the service. Their roles included:

What did we do?
In October 2017, the NHS, Local Authorities and the Brain Charity worked in collaboration to pilot a monthly drop-in clinic entitled the Life Link clinic and was based within one of the complex rehabilitation inpatient units within Merseyside. The pilot site was evaluated pre and post implementation between December 2018 and May 2019. The Life Link clinic went on to be replicated on four other complex rehabilitation units and a further two sites were identified for adoption of the Life Link model. The team gained support from ARC NWC and public advisors to offer guidance on the implementation and evaluation of the project.
Prior to the implementation of the Life Link clinic at the two new sites, semi-structured interviews were carried out with staff and service users to evaluate the existing three services and improve implementation of the two new sites. A staff questionnaire was also randomly sent to 30 staff members and 22 were returned. Using the bespoke questionnaires, the Depression, Anxiety and Stress Scale (DASS-21) and the NHS family and friends test, service users were asked to provide feedback on the service and rate their levels of stress and anxiety before and after accessing the service.
What we found and what does this mean?
Results from the 22 questionnaires completed by staff pre-implementation showed that 77% of staff strongly agreed that trying to support patients and their families with socioeconomic issues significantly impacted on their clinical treatment time, reinforcing the need for the service.
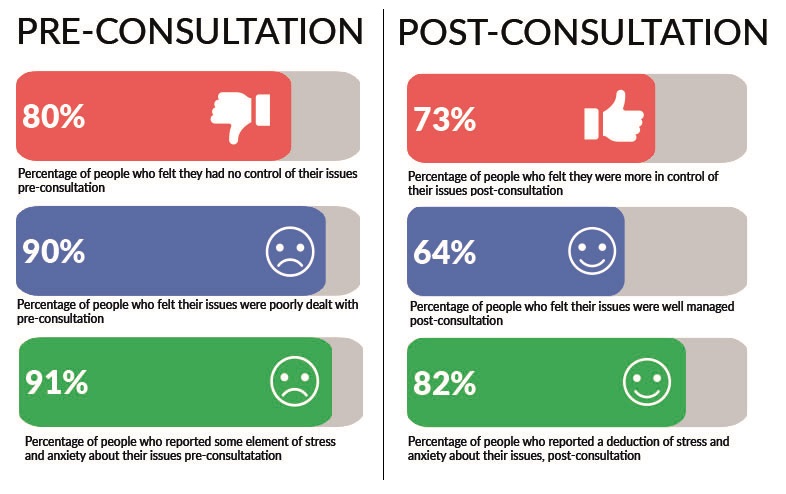
Pre and post consultation, users of the Life Link Clinic were asked to rate how well they felt their issues were managed. Pre-consultation, 90% of participants felt their issues had been poorly managed. However, post-consultation, 64% of respondents felt that their issues were very well managed and further 27% felt they were slightly well managed. The service also impacted on the level of control that users felt they had over their issues as well as the level of stress and anxiety they felt. Pre-consultation, 80% of users felt a loss of control of their issues, in comparison to 73% who felt more in control post-consultation and 82% of participants reported a reduction in feelings of anxiety and stress following a discussion at the clinic. Analysis from the semi-structured interviews identified time as a recurring theme both as a facilitator and a barrier to using the service. The clinic would free up staff time for clinical treatment but conversely it was felt that the clinic maybe difficult to access due to the times it is facilitated. However, users also felt that the clinic was beneficial and gave them peace of mind knowing that their issues were being sorted out and letting them focus on their rehabilitation.
The small service evaluation provided evidence that the provision of support to patients and their families with socioeconomic needs who have been inpatients rehabilitation units is beneficial. It appears to reduce stress, anxiety, and increases a feeling of control over these issues, providing peace of mind to both the patient and their families. From a staff perspective, the service provides a more effective use of clinical treatment time.
Wider impact on health inequalities/health equity
The Life Link clinic can provide individuals and their families with the knowledge and support to access welfare and benefits advice, housing channels, employment rights advice, and give carers advocacy to challenge decisions that affect them. This can provide empowerment to the users of complex rehabilitation inpatient and community services and potentially reduce the health inequalities they encounter.
The support provided by the Life Link clinic could also have a wider impact within acute hospital care. Prior to the implementation of the Life Link clinic, clinicians time was consumed by trying to support patients and their families with non-medical issues impacting on the amount of time dedicated to clinical treatment. Therefore, having a service dedicated to providing socioeconomic support could improve rehabilitation outcomes and be a more effective use of a clinician’s time which could contribute to a reduction in delayed discharges. Additionally, the Life Link service could also help create a cultural shift from a focus on disease to adopting a more holistic approach focusing on the multiple factors that affect health.
The Life Link model could also be adapted to other areas and interest has been expressed by other populations which experience similar health inequalities such as those with learning disabilities and dementia.
What next?
COVID-19 did have an impact on the delivery of the Life Link clinic, however there are plans to reintroduce the clinics with opportunities for families to access the clinic via a virtual platform. Future steps also include the formulation of a business plan to enable sustainable funding and two further adoption sites in two different organisations have been identified with partners of the Cheshire and Merseyside Rehabilitation Network.
With the assistance of ARC NWC, the team successfully submitted an abstract at the 2nd Annual UK Implementation Science Research Conference, ‘Advancing the science of scaling up: Improving efficiency and effectiveness of implementation strategies in healthcare’ in July 2019 (6). Findings were also presented at the NIHR ARC NWC Partner Priority Programme showcase event, also held in July 2019 (7). Working in conjunction with the public advisors, the project management team are in the process of contributing to a book chapter with the intention of providing an insight into the journeys faced by patients undergoing complex rehabilitation and the challenges that they, and their families face in respect to health inequalities. Led by ARC NWC, there are plans to produce an academic paper for journal publication.
This project was led by Claire Hendry from the Cheshire and Merseyside Rehabilitation Network and her team which consisted of the following: Clare Moore (Matron), Jenny Bailey (Public Advisor), Peter Bailey (Public Advisor) Jessica Hopkins (Rehab Coordinator), Maria Moyo (Social Worker), and Margaret Dickinson (The Brain Charity). This research was supported by the National Institute for Health Research Applied Research Collaboration North West Coast (NIHR ARC NWC). This case study was created by Paul Boland, MSc, a Research Assistant from the University of Central Lancashire and member of the MIDAS team (Evidence Synthesis) in collaboration with the project lead.
References:
1. Jagnoor J, Cameron I. Traumatic brain injury – support for injured people and their carers. Australian Family Physician. 2014;43:758-63.
2. The Neurological Alliance. Neuro Patience: Still waiting for improvements in treatment and care. 2019.
3. Liverpool City Council. The Index of Multiple Deprivation 2019: A Liverpool Analysis. 2019 [Available from: https://liverpool.gov.uk/media/1359213/imd-2019-liverpool-analysis-main-report.pdf]
4. NHS England. Neurological Conditions. 2021 [Available from: https://www.england.nhs.uk/ourwork/clinical-policy/ltc/our-work-on-long-term-conditions/neurological/].
5. Humphries TJ, Ingram S, Sinha S, Lecky F, Dawson J, Singh R. The effect of socioeconomic deprivation on 12 month Traumatic Brain Injury (TBI) outcome. Brain Injury. 2020;34(3):343-9.
6. Proceedings from the 2nd Annual UK Implementation Science Research Conference, ‘Advancing the science of scaling up: Improving efficiency and effectiveness of implementation strategies in healthcare’: meeting abstracts. Implementation Science. 2019;14(S2).
7. Henry C, Giebel, C., Villanueva, T., Hill, N., Spearitt, T., Johnson, L., Moore, C., Smith, J., Mealey, S., Bailey, P., Bailey, J., Burnage, H., Huges, M., Mayo, M., Osman, H. Meeting the socio-economic needs of patients and their families in complex rehabilitation – The Life Link clinic. 2019. [Available from: https://www.clahrc-nwc.nihr.ac.uk/media/Info%20Hub/Claire%20Hendry%20-%20Walton%20Centre.pdf]