Regional inequalities in the impact of the COVID-19 pandemic
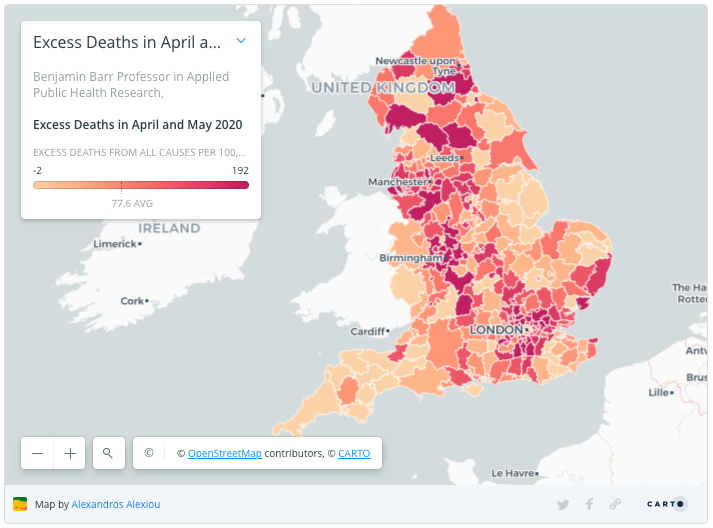
Are some places more equal than others? In this blog, ARC NWC staff Dr Tanith Rose, Dr Alexandros Alexiou, Dr Konstantinos Daras & Professor Ben Barr explore the regional inequalities in the impact of the COVID-19 pandemic. See accompanying interactive map here.
Reports that politicians, celebrities and members of the royal family have been diagnosed with COVID-19 have prompted some to portray the disease as a great equaliser, which can affect even the most privileged. The impact of COVID-19 has in fact certainly not been equal. Some communities have experienced much higher rates of infection and mortality. Whilst London was initially the most effected region, the North West, North East and the West Midlands now have the highest rate of excess deaths due to the pandemic.
Some of the variation between places in the UK, in the first wave, was related to initial importations of cases from elsewhere in Europe and the dynamics of transmission between places following key transport links. It is increasingly clear, however, that ethnic and socioeconomic inequalities are playing a large role in explaining regional variations in the impact of COVID-19.
Our research explored the relationships between ethnicity, deprivation and COVID-19 mortality at local authority level in England, and revealed stark ethnic and socioeconomic inequalities in mortality rates. Local authorities with a greater proportion of residents from ethnic minority backgrounds had higher COVID-19 mortality rates, as did places with a greater proportion of residents experiencing deprivation relating to low income. These associations were independent of each other, and remained after controlling for population density, the duration of the epidemic and the proportion of older residents.
Ethnic minority and socioeconomically disadvantaged groups may be at greater risk of exposure, susceptibility and severe consequences from COVID-19 due to overcrowded housing, employment in essential occupations, reliance on public transport, unequal access to effective healthcare and higher prevalence of chronic illnesses.
Now is the chance to learn from the first wave and put in place control measures to better protect those communities. What is needed is an approach that is tailored to the communities most at risk and led by local government in partnership with these communities. An approach that has been effective in Ceredigion in Wales, for example, which has experienced very low diagnosis and mortality rates compared to the rest of the UK. The strategy followed by the UK government so far has been centrally led and outsourced often bypassing local public health teams. This one-size fits all approach is unlikely to address the stark inequalities that COVID19 has revealed. The initial strategy was to rely on an app for much of the contact tracing, although this has now been delayed due to technical difficulties, it was always likely to exacerbate the unequal risk of COVID19. Resources need to be targeted to those communities most at risk, however the allocation of resources to local areas so far has not clearly taken into account the key drivers of needs related to COVID19.
It is likely that a second wave of the pandemic is coming, and we have a few months to get communities “second wave ready”. It is also likely that a second wave will hit the most disadvantaged communities first and hardest – leading to even starker inequalities than in the first wave To highlight the distribution of vulnerability across England we generated a neighbourhood level vulnerability index for COVID-19 mortality, identifying those areas that are likely to be most vulnerable in a second wave as they have higher numbers of people from Black Asian and Ethnicity Minority (BAME) groups, living in poverty, over 80 years old, having a chronic health condition, living in a care home and/or living in overcrowded housing For example – targeting a national fund to reduce vulnerability, implementing systems of active case finding in high risk groups and communities and building resilience in the most
disadvantaged places. Our findings indicate that communities with high levels of vulnerability to COVID-19 are clustered within the North West, West Midlands and North East regions.
We need to act now to protect these communities if we are to prevent further avoidable deaths this winter. For example – targeting a national fund to reduce vulnerability, implementing systems of active case finding in high risk groups and communities and building resilience in the most disadvantaged places.