The predictive capability of SAVI index for COVID19
This blog originally featured on the Liverpool and Lancaster Universities Collaboration for Public Health Research (LILaC) website.
The Small Area Vulnerability Index (SAVI) is an empirically informed measure of COVID-19 vulnerability for the 6,789 Middle Super Output Area (MSOA) in England. The SAVI index investigates the association between four predictors (proportion of the population from Black, Asian and Minority Ethnic (BAME) backgrounds, living in care homes, living in overcrowded housing and having been admitted in the past 5 years for a long-term health condition) and COVID-19 mortality as occurred in England between 1 March and 31 May 2020.
Our findings indicated high levels of vulnerability to COVID-19 have been clustered within the North West, West Midlands and North East regions and we highlighted the need for control measures and policies to shield certain groups to take into account these factors targeting resources and proportionate to the greater needs experienced by some communities.
To further explore the predictive capability of the index, we illustrated the association between the COVID-19 deaths per 10,000 people in the second wave (1 June – 31 December 2020) and the SAVI index. The figures below shows that twice as many deaths have been recorded during the second wave in most vulnerable communities (high SAVI score).
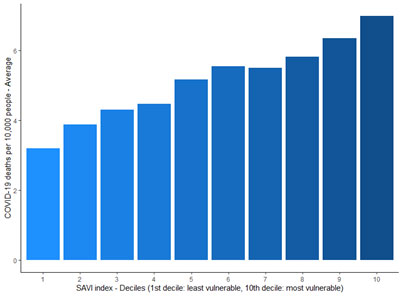
Also, we used a Poisson regression model to investigate the association between the COVID-19 mortality in the second wave and the SAVI index. The SAVI index was contracted to reflect the relative increase in mortality risk, in other words a SAVI of 2 reflected an estimated doubling of mortality risk in the first wave. The Poisson regression analysis shows that unit increase in the SAVI index was associated with a 60% increase in the COVID-19 mortality rate (incidence rate ratio, IRR 1.60, 95% CI 1.49 to 1.72, p<0.01). This suggests that the SAVI was a reasonable predictor of mortality risk for small areas in the second wave.
There remains considerable uncertainty related to the extent to which factors increase vulnerability, however, the SAVI provides an initial starting point for public health agencies to investigate further in combination with other local intelligence in identifying and mitigating risks in vulnerable communities. Many of the risk factors included in the SAVI are also associated with low vaccine uptake. Strategies for promoting vaccine uptake should target places with greater vulnerability in combination with low vaccine uptake by engaging and offering practical support to those communities.
Dr. Konstantinos Daras and Prof. Benjamin Barr
Department of Public Health, Policy and Systems
Institute of Population Health
University of Liverpool